Hidradenitis suppurativa
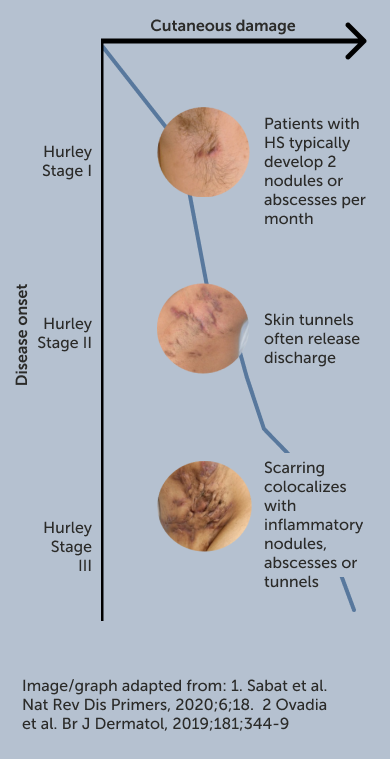
Hidradenitis suppurativa (HS) is a debilitating, chronic inflammatory skin disease characterised by persistent and painful cutaneous nodules, abscesses and draining tunnels.
Areas commonly affected include the axillary, anogenital, inguinal and perianal/gluteal areas. Over time, chronic uncontrolled inflammation results in irreversible tissue destruction and scarring.1

What’s the bigger picture in HS?
Listen to this Under The Skin podcast which welcomes Dr Barry McGrath, HS patient advocate and co-founder of patient association HS Ireland, and Dr John Ingram, HS Consultant Dermatologist at Cardiff University, to share an overview of what HS is, its presentation in patients, epidemiology and global prevalence.
Epidemiology
HS affects approximately
of the UK population2 and the average age of disease onset is
HS is approximately 3x more common among women than men4 and notably more common in those with skin of colour (0.30%) versus those with Caucasian ethnicity (0.09%).5
What are the symptoms that patients commonly struggle with?
Understand how HS affects day-to-day life with this helpful synopsis.
Common risk factors
Smoking:
HS incidence among tobacco smokers is ~2x the rate of non-smokers.6
Obesity:
Body mass index (BMI) is significantly higher in people living with HS versus the general population.7
Genetics:
Up to 38% of patients with HS have a family history of HS.8
It is important to note that when having discussions about lifestyle modifications, such conversations should be tactful and diplomatic.
Patients with HS have described discussions about weight and smoking as leading them to feel:9
Shame Stigmatised Dehumanised
How should I approach difficult conversations about lifestyle with patients?
Watch Dr Barry McGrath, HS patient advocate and co-founder of patient association HS Ireland, provide advice on how dermatologists can better support patients during delicate consultations in this video.
View the patient conversation tool kit.
Burden of HS
HS profoundly impacts quality of life and may carry a higher patient burden than other chronic inflammatory skin conditions, such as psoriasis.10
“What happens is the pain increases and then you get to the point where it’s the most unbearable thing you could imagine”9
The highest proportion of physical disability is thought to arise from the soreness and pain associated with the disease.14 However, purulent discharge, malodour and disfigurement also contribute to the burden and can result in isolation and fear due to stigmatisation in work and personal life.10
“There are days when I can’t hold up my arm to tie up my hair…it’s little things like that or even climbing the stairs.”9
This can have devasting impact on those affected and is associated with high unemployment, slower income growth, and a higher risk of leaving the workforce:
days mean work absence annually amongst employed HS patients15
of patients with HS report workplace absences as a result of their disease15
of patients with HS are unemployed vs. 5% in the general population1
Listen to the second episode in the Under The Skin series
Professor Falk Bechara, the Head of the Department of Dermatologic Surgery at the Ruhr University Bochum, Germany, and Dr Barry McGrath, HS patient advocate and co-founder of patient association HS Ireland, discuss the profound physical, psychological and social impacts that HS can have on a patient’s quality of life.
View the patient conversation tool kit.
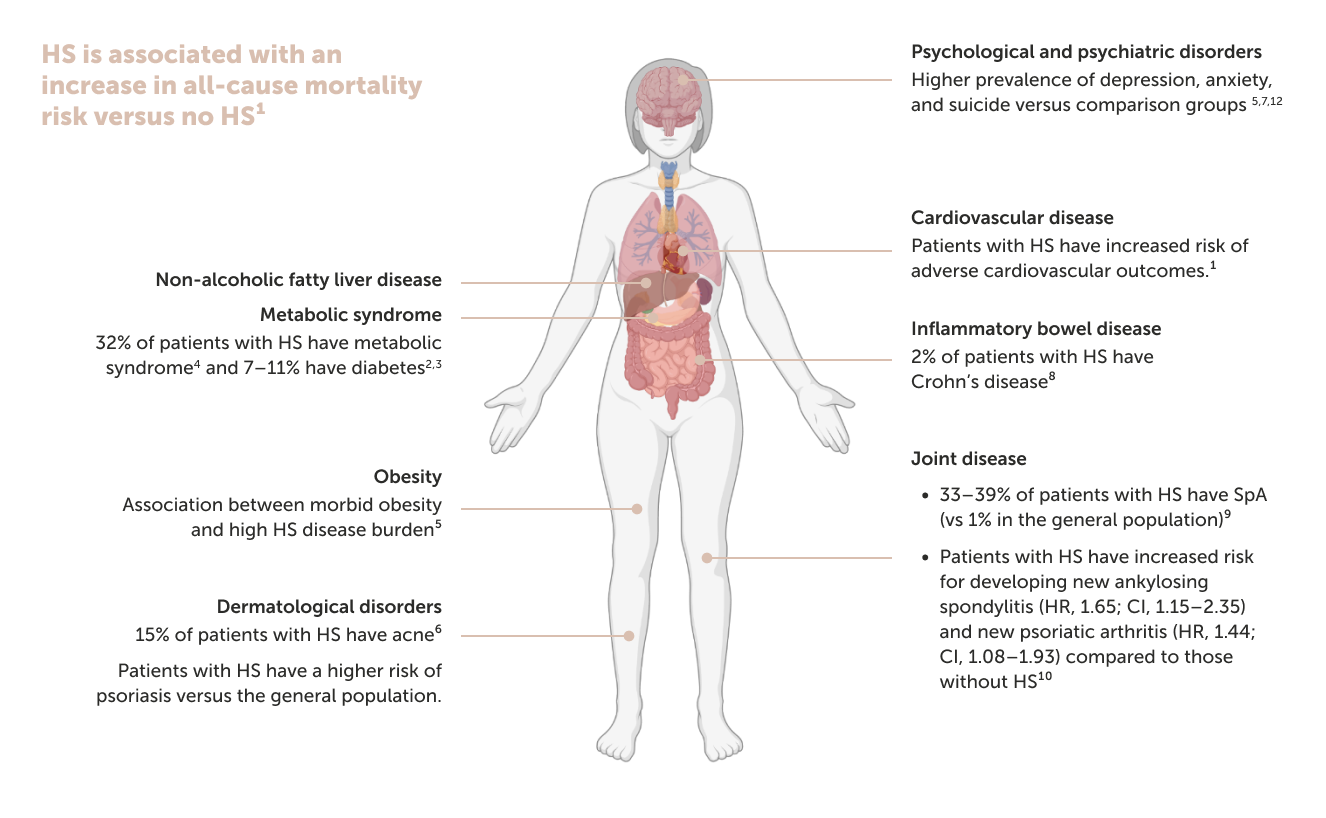
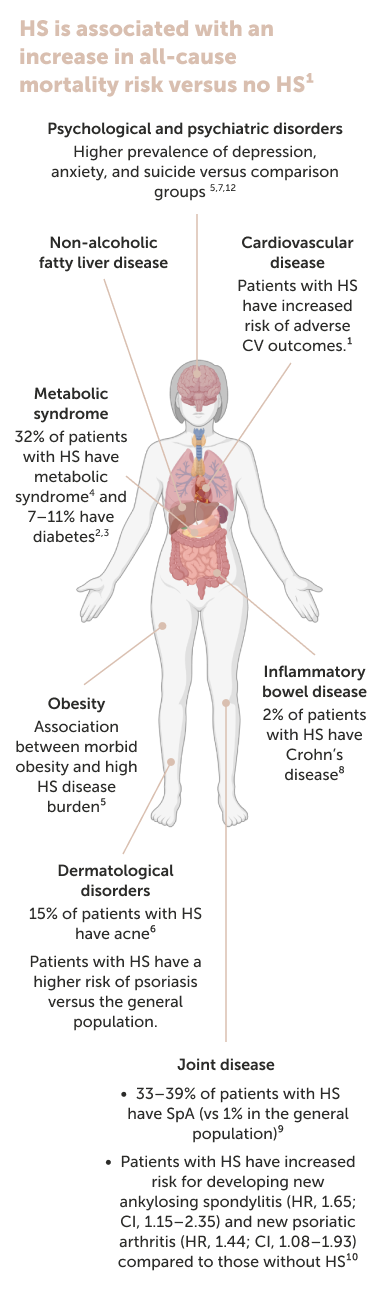
Comorbidities
Patients with HS face a high burden of comorbidities.
Given that persistent inflammation in HS can accelerate disease progression and a greater risk of developing comorbidities, it is critical to resolve inflammation as early and as completely as possible.
Listen to the Under The Skin podcast to understand the bigger picture in HS.