Timely and accurate diagnosis
People living with hidradenitis suppurativa (HS) face a diagnostic delay of at least 7 years,1 and over 70% of patients are already exhibiting moderate to severe disease when first diagnosed.2
Potential reasons for delays in diagnosis…
Lack of knowledge and awareness in the medical community2
Under-recognition in specialities other than dermatology3
Patients face socio-economic barriers3
Feelings of shame may cause people to hide their HS from their support network4
Disease-related stigma may cause patients to delay seeking medical help5
How can we bridge the gap between general practice and dermatologists?
Watch Dr Angelika Razzaque, a GP with a specialist interest in dermatology, share how dermatologists can help GPs provide better care for.
Learn what UCB is doing to raise the standard of care in HS.
Caring with compassion
Positive body image and self-esteem may be a challenge for some people living with HS, and the first consultation may be the first time a patient has shown intimate areas to an healthcare professional or to any other person.
“I used to bawl my eyes out. I used to cry. You know, you'd come back after going to the doctors and you cry because they just don't realise.”6
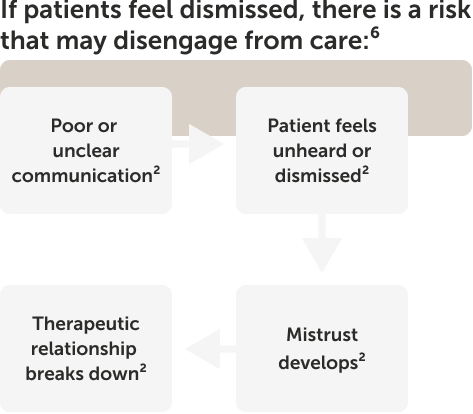
What can I consider when discussing HS with patients?
View the patient conversation tool kit.
Listen to the second episode in the Under The Skin series, where Dr Barry McGrath, HS patient advocate and co-founder of patient association HS Ireland, and Professor Falk Bechara, the Head of the Department of Dermatologic Surgery at the Ruhr University Bochum, Germany, discuss the profound physical, psychological and social impacts that HS can have on a patient’s quality of life.
LISTEN NOW
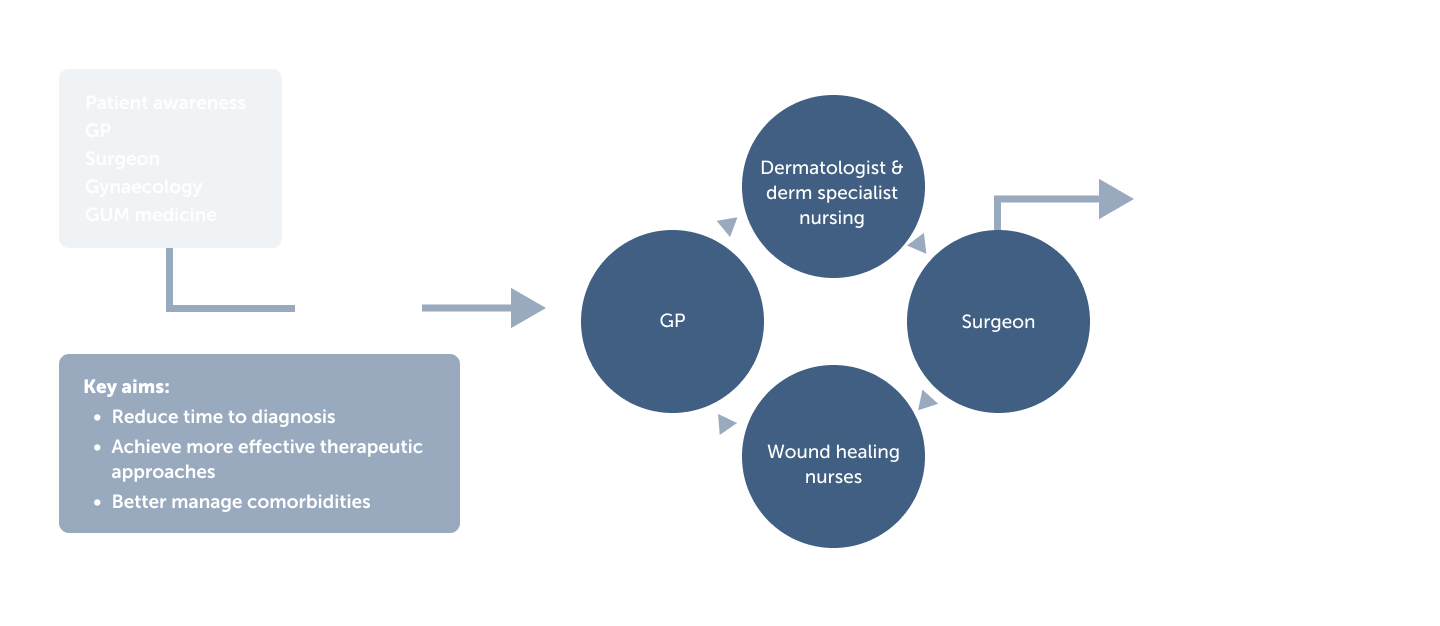
The role of the
multidisciplinary team
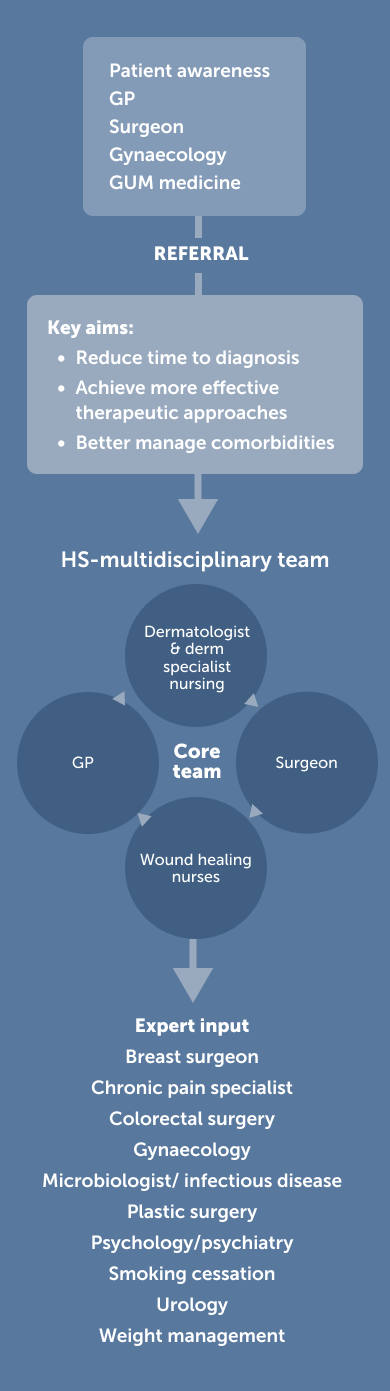
It has been proposed that multidisciplinary teams are needed for the optimal management of HS. The aims of such teams are to reduce the time to diagnosis, achieve more effective therapeutic approaches through an informed collaborative approach, and better manage the numerous comorbidities for which patients with HS are at risk.7,8
Learn what UCB is doing to raise the standard of care in HS.
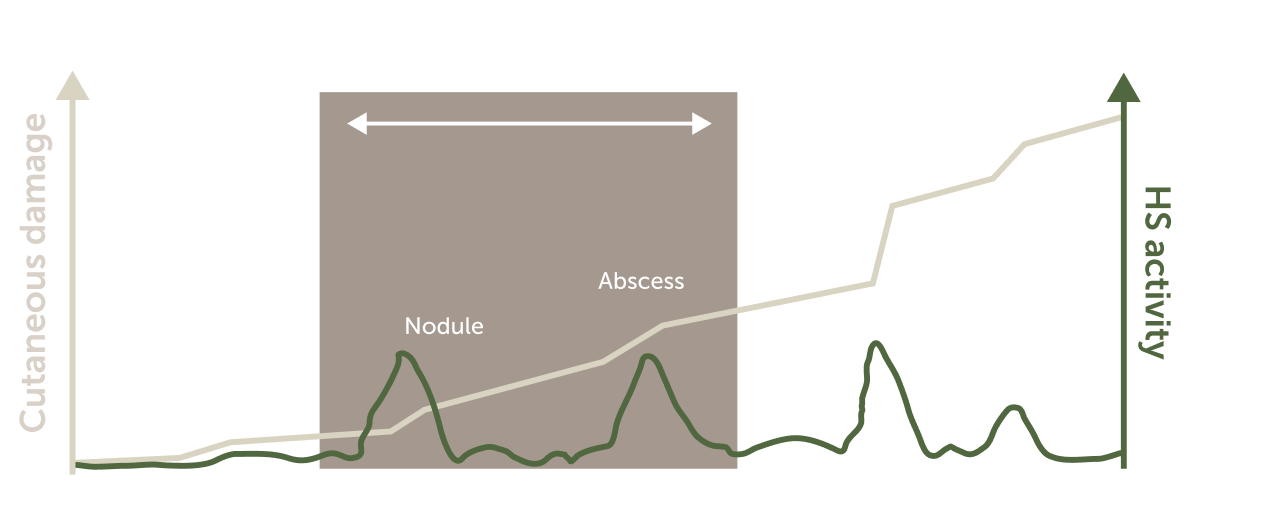
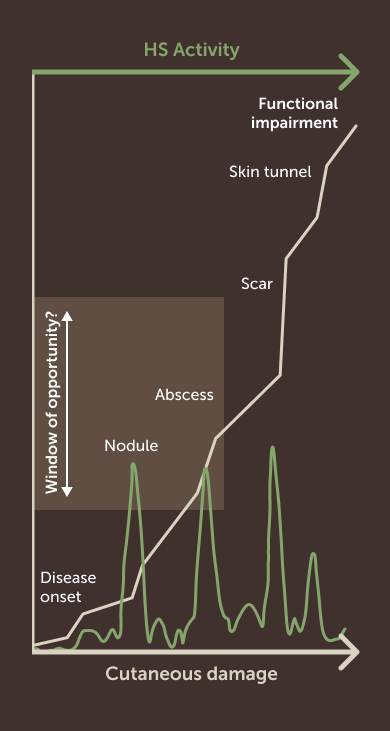
Managing patients within a therapeutic ‘window of opportunity’
Uncontrolled disease progression in HS is a consequence of delayed diagnosis and/or ineffective treatment. Uncontrolled disease results in significant tissue destruction, functional impairment and adverse outcomes including:
- Greater risk of suicide9
- Impaired response to treatment10, 11
- Working disability because of active lesions11
- Continued formation of tracts and scarring12
- Increased risk of depression, fatigue and an impact on ability to work11, 9, 13
- Further shame and psychological distress for the patient4
Timely initiation of therapy is key, suggesting that there is a therapeutic ‘window of opportunity’ in which healthcare professionals should seek to initiate effective treatment:14
Watch Dr John Ingram, Dr Angelika Razzaque and Dr Barry McGrath discuss the value of capturing patient outcomes in clinic.
Download a guide to assessing HS disease severity and progression.
Explore with Dr John Ingram, Consultant Dermatologist, the concept of the therapeutic window of opportunity, why new treatment options are needed and what this may mean for HS guidelines.