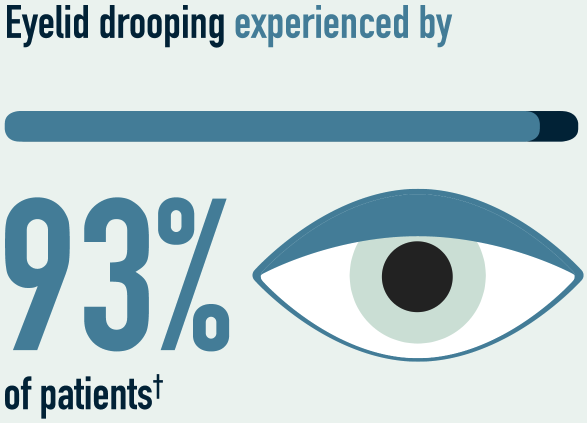
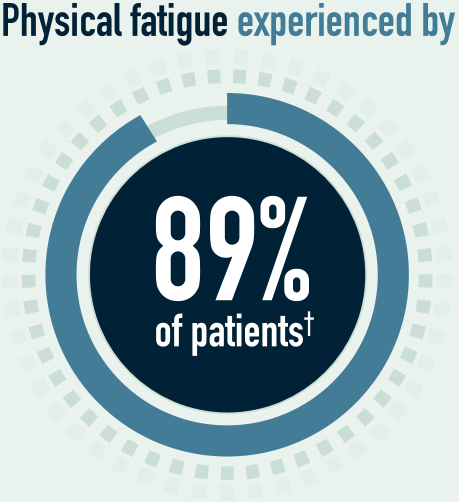
non-interventional study, those most frequently reported were:2
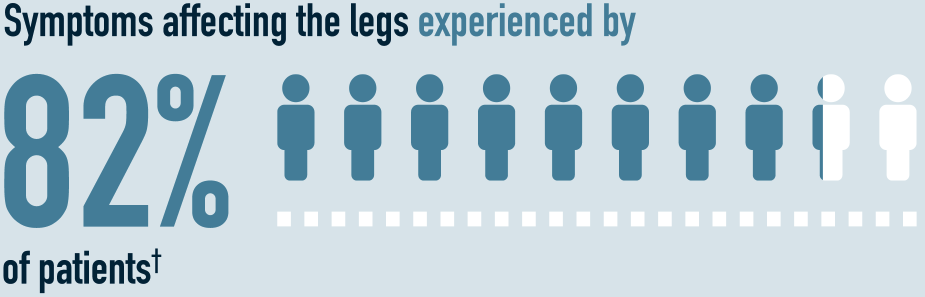
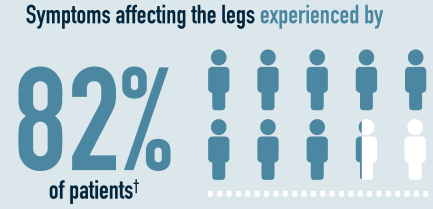
For patients with gMG, instability and unpredictability are ever present, and nearly all patients experience symptom fluctuations severe enough to influence their daily life2–6†
The systemic side effects of long-term corticosteroid therapy are numerous and can be highly impactful8
Intravenous immunoglobulin (IVIg) treatment has been a mainstay of myasthenia gravis (MG) treatment for decades, but limitations remain, such as time-intensive, shortages can occur, slow therapeutic onset and inadequate symptom control9–12
Around 80% of patients do not achieve stable remission, and 10% are intolerant to current treatments such as acetylcholinesterase inhibitors (AChEIs), immunosuppressive agents and thymectomy13
Patients fear experiencing a myasthenic crisis; for 15–20%, this fear becomes a reality7,14
The unmet need for targeted immunomodulatory drugs for the treatment of MG has resulted in an ongoing campaign to develop safer and more effective treatments10
Although some triggers of intermittent worsening of symptoms have been identified, they are not well understood and are often beyond a patient’s control3,6,15
Triggers include:6,15
Mental or
physical stress

Changes in the weather
Infections
Certain drugs

Vaccinations

Multiple studies have found that people with gMG are in a constant state of adaptation to cope with fluctuating and unpredictable muscle weakness4–7
Achievement of minimal manifestation status within the first 12–24 months of treatment initiation is associated with improved long-term outcomes, more sustained control of symptoms, and reduced risk of exacerbations and myasthenic crises16-18
Patients who still experience symptoms 24 months after disease onset despite immunosuppressive therapy are less likely to achieve disease control without modification of therapy16
Law et al, 2021. The lived experience of myasthenia gravis: a patient-led analysis
Led by a Patient Council of nine individuals living with MG, this analysis reviewed insights from multiple data sources with the objective of generating a series of statements that best represent the lived experience of gMG7
References